Abnormal changes in the cartilage and bones of the spine lead to the development of the disease, which, according to the ICD-10 code, refers to the localization of M42 and is called thoracic osteochondrosis. The middle part of the spine is less stressed than the spine and neck, but the deformities are difficult to heal. Due to the rounded configuration of the sternum, the load is unevenly distributed, osteophytes and other dysplastic manifestations are visible.
Symptoms and signs
The disease occurs in the pulpous nucleus of the intervertebral disc, spreads to the fibrous fibrous ring and other parts of the spinal segment, which provides mobility of the spine. The changes are manifested by compression, reflex or mixed neurological disorders and syndromes.
The pain manifests itself with physical force. There are different types of feelings:
- mild long-lasting pain in the thoracic region is called dorsalgia;
- acute and severe colic, causing a difficult inhalation or exhalation, causing muscle inactivity - dorsago.
The symptoms and treatment of thoracic lumbar osteochondrosis depend on the degree of wear and tear of the bone apparatus and the generalized and local stage of aging.
Symptoms include:
- damage to peripheral nerve processes (neuralgia), characterized by painful attacks along the intercostal vasoconstrictors;
- concentration of pain on the left side of the chest or the appearance of strong painful sensations of a shingles nature;
- decreased mobility of the spine in the thoracic region;
- numbness in the arms and hands;
- decreased sexual function;
- the appearance of pain in the region of the internal organs, can give the heart, stomach, liver;
- a lump in the neck, cheekbones, and head, lumbago, cough, or sore throat;
- arrhythmia, tachycardia, fever.
The symptoms of osteochondrosis are masked as a manifestation of related diseases, so the symptoms are ambiguous. The spinal nerves are concentrated around the spinal column; When they are compressed, signals are sent to various parts and organs of the body.
Causes of osteochondrosis
There is no exact information about the factors that deform the intervertebral discs. A common cause of osteochondrosis is scoliosis or curvature of the spine, which is more common in childhood and adolescence.
The theory takes into account the following factors of vertebral deformity:
- dysontogenetic;
- hormonal;
- vein;
- functional;
- attractive;
- infectious;
- immune;
- dysmetabolic;
- mechanics;
- irsi.
Deterioration and aging of bones and cartilage occur as a result of previous exposure to adverse conditions. Atrophic degenerations in the spine are predetermined by a genetic factor, and a disease with clinical symptoms occurs under the influence of exogenous and endogenous environments.
The result in the form of complications in the work of the spine occurs when the process of destruction of complex substances takes precedence over their synthesis. Exacerbation occurs when the disk power supply is disrupted and there is a lack of useful elements. The penetration of elements and dissimilation products decreases, cell viability decreases, and parts of cells accumulate due to self-destruction. The production of complex proteins is reduced, collagen fibers are destroyed.
The mechanical effect on the formation of the annular joint is intensified, the layered structure is irregular, the fibrous skeleton is torn. The disc is crushed under the influence of biomechanical factors and body movements, the ability to fix is reduced. Blood vessels and nerves can grow into the annulus due to a decrease in hydrostatic pressure.
Diagnostic methods
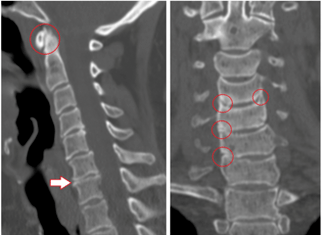
Radical, painful, reflex, myotonic, vegetative and vascular factors are identified in the recognition process. It is difficult to determine the best method of examination, because in each case the diagnosis is made individually.
The main methods are:
- X-ray diagnosis;
- CT scan;
- Magnetic resonance imaging.
X-ray analyzes the condition of the spine, images are given in oblique, lateral and direct projections. Sometimes a person bends, twists, or leans to the side for a photo.
Contrast radiography is divided into the following studies:
- pneumoelography - 20 to 40 ml of air is injected into the spinal canal;
- angiography - 10 ml of contrast agent is injected into the vertebral lumen and 7 to 9 images are taken in 2 - 3 seconds;
- myelography - injection of staining fluid into the subarachnoid lumen, followed by transillumination of the structure;
- discography - the stained substance is injected directly into the disc for local examination.
Computed tomography assesses the structure of bone and tissue, the condition of blood vessels. The painless method takes three-dimensional images in a matter of minutes.
Advantages of CT:
- high detection speed;
- inspection of "dumb" areas during motion diagnostics;
- the possibility of multispiral angiography;
- Recognition of long objects by obtaining high-quality low-thickness cuts.
MRI uses the magnetic field of a machine that builds hydrogen atoms in the human body in parallel with motion. The particles signal, the reaction is recorded. The tomograph recognizes the waves and displays the result on the screen. There is no radiation with MRI, the method is less dangerous, but is not recommended for pregnant women.
Treatment and prevention
Osteochondrosis needs to be treated in several stages, the complexity of which depends on the severity of the disease, contraindications and body resources.
Methods:
- medicines and drugs;
- physiotherapy methods, exercises to remove the clamps, to alleviate the patient's condition;
- operation.
There is a direction of kinesitherapy, within which it is possible to treat problems of the spine in the form of hernias, spondylosis with restorative gymnastics. Postoperative recovery has also been developed.
Yoga exercises help adult men, women and children to relieve pain, warn that the main thing is a psychological attitude.
Medications
Medications are prescribed by a neurosurgeon or neurologist according to the card and medical history. Patients take medication in the hospital or at home, the main thing is to follow the instructions and do not go beyond the reception regimen.
Common medicines:
- NSAIDs relieve pain, fever and inflammation;
- muscle relaxants reduce skeletal muscle tone;
- hormones reduce neuralgic pain;
- Vitamins B2, B6, B12, A and C are taken during remission and for simple prophylaxis;
- diuretics eliminate swelling and relieve constricted radicular nerves;
- neurometabolic stimulants improve metabolism in nerve tissues;
- Chondroprotectors restore the cartilage of the vertebrae after damage.
Sometimes the patient is without medication in the first stage of the onset of unpleasant feelings. It is enough to exercise and use massage.
Physiotherapy

Such exposure is used in combination with drug therapy or separately. In addition, bed rest is applied, heat is applied to the affected area. Folk recipes are used to relieve pain.
Physiotherapy procedures at a medical facility include:
- ultrasound and phonophoresis;
- shock wave therapy;
- detensor effect;
- laser therapy;
- electrotherapy;
- magnetic waves;
- mud therapy and balneotherapy;
- massage.
Ultrasound covers the effects of high-frequency waves on tissues, reducing pain sensitivity. With ultrasound, painkillers and anti-inflammatory drugs are added for better delivery to the affected areas.
Shock wave therapy is the transmission of acoustic waves to the painful area, used to improve blood circulation and speed up metabolism. Detensor therapy involves stretching the spine using the patient's body weight.

Laser therapy is based on the helium-neon generation of lasers to activate bioelectric currents in nerve fibers. The laser affects the inflamed nerve roots in the paravertebral region along the thoracic region.
Electrotherapy improves tissue nutrition and metabolism in tissues, and pulse currents affect nerve endings. Low-frequency waves relieve acute pain and are used as first aid.
Magnetic therapy is used to relieve swelling, spasms and inflammation. A magnetic wave inductor is placed in the affected thoracic region. Balneotherapy and mud treatments include swimming in the pools, taking a bath, and contrasting showers for treatment and recovery. Metabolism is normalized, blood flow to the affected areas is accelerated, pain and inflammation are reduced.
Therapeutic massage for osteochondrosis of the thoracic spine is vacuum, point and lymph drainage, improves blood microcirculation, tissue nutrition and tones muscles. Sessions are conducted by an authorized specialist, and if you entrust the spine to amateurs, dangerous results can occur. Massage is prescribed after the end of the acute phase, the first session should not exceed 10 minutes.
Surgical treatment
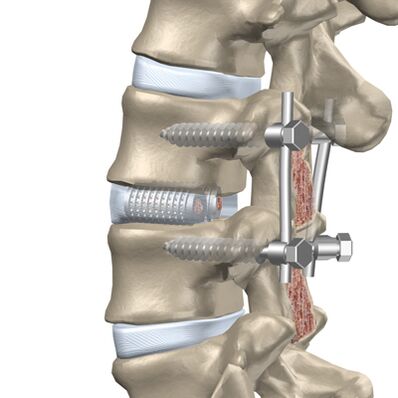
If medical treatment, massage and other procedures do not alleviate the condition, the patient is indicated for surgery.
The intervention is divided into 2 stages:
- elimination of the cause of severe pain (decompensation);
- stabilization of the spine.
Facetomy is performed with a posterior approach, because the facet joints can compress the nerves. A foraminotomy is an enlargement of the radicular canal through which the nerve exits the vertebrae. Laminectomy removes the back of the vertebra, which protects the lumen of the spine and compresses the brain due to deformation. Laminotomy involves widening the canal opening where the spinal cord is located, as well as removing a separate part of the back of the vertebrae.
Anterior surgery is performed if there is a protrusion (bulge of the spinal disc towards the spinal lumen) or when the hernia protrudes into the canal.
The following methods are used for anterior decompression:
- discectomy - removal of the entire disc or a separate part of it;
- Corpectomy - removal of an entire vertebra and an adjacent disc, followed by implantation.
Discectomy and corpectomy lead to destabilization of the column and increase the risk of neurological defects. Rigid fixation or fusion of three vertebrae is used.
Prevention of thoracic osteochondrosis

Exacerbation of the disease reduces the ability to work and the quality of human life, so special attention is paid to prevention. As a result, vertebral degeneration appears late and disability is avoided.
Methods of disease prevention:
- decreased physical activity in the spine;
- you can not stand for a long time without changing the supporting member, you can lean on the improvised object or wall;
- it is not recommended to sit at a desk for a long time and to take active breaks while working on the computer, to walk around;
- mattresses and orthopedic headrests are selected for sleeping;
- avoid sudden turns and jumps while running and walking, walk in shoe-absorbing shoes with small heels;
- Carry weights not exceeding 10 kg, gradually lift from the sitting position.
You must use supports for the rear and headrests in the car, and the driver's seat must be rigid. The work cannot be done in a semi-bent position, you can stand or sit. Well-developed muscles support the skeleton, so focus on possible physical training and hardening.
Possible complications
The disease develops over a long period of time, sometimes the symptoms of pain do not come immediately. Any degenerative changes in the thoracic region lead to the appearance of pathologies.
Types of complications:
- cardiovascular pathology with subsequent myocardial infarction or angina pectoris;
- inflammation of the peripheral nerves with intercostal neuralgia or chest pain from compression of the roots;
- protrusion of intervertebral discs.
Complications occur with advanced forms of osteochondrosis, so timely treatment in the early stages will help prevent concomitant diseases.

























